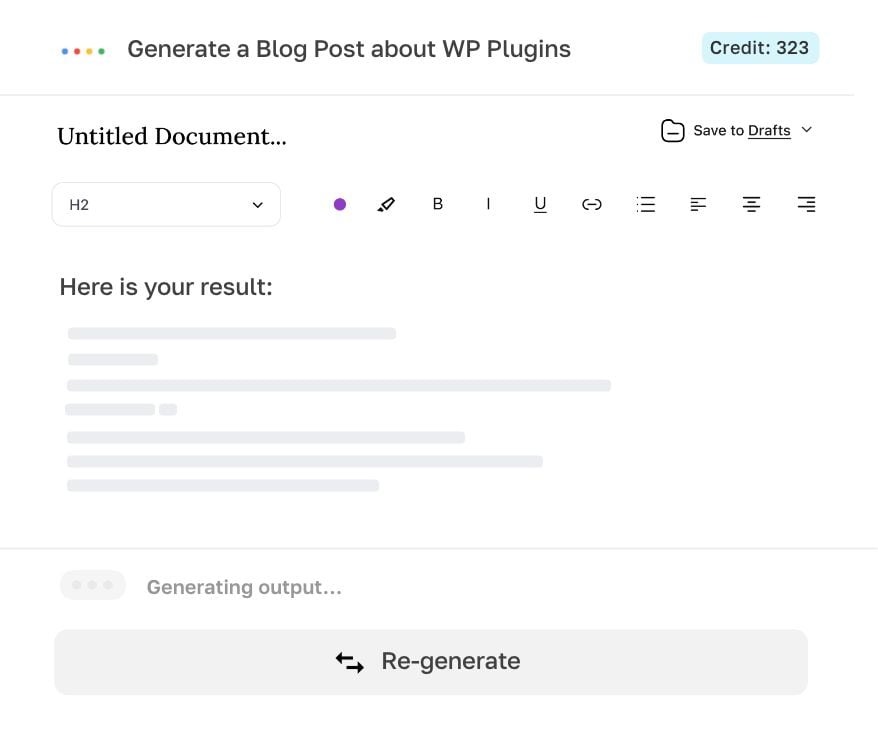
Say goodbye to writer's block AI
Intelligent Writing Assistant
Writer is designed to help you generate high-quality texts instantly, without breaking a sweat. With our intuitive interface and powerful features, you can easily edit, export, or publish your AI-generated result.
Generate, edit, export.
Powered by OpenAI.